Ebola virus disease
Foot Ulcers In Diabetes: Simple Guide For Diabetics With 5 Practical Tips To Prevent Foot Ulcers
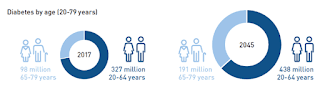
Diabetes prevalence in India has increased steadily since 1990, notably surging after 2000 while the 2023 ICMR INDIA B study by the Indian Council of Medical Research indicates that around 101 million people in India have diabetes. India ranks second globally in the diabetes epidemic, projected to rise to 27.5 million among those aged over 65 by 2045 as alarmingly, around 57% of diabetic cases go undiagnosed, totaling approximately 43.9 million.
 Foot ulcers in diabetes: Simple guide for diabetics with 5 practical tips to prevent foot ulcers (Photo by Alex Huge)
Foot ulcers in diabetes: Simple guide for diabetics with 5 practical tips to prevent foot ulcers (Photo by Alex Huge) Diabetes-related foot complications pose a significant morbidity risk due to social and economic factors. Additionally, delays in accessing healthcare exacerbate the issue, with many patients consulting informal providers initially.
HT launches Crick-it, a one stop destination to catch Cricket, anytime, anywhere. Explore now! Understanding Diabetes-Related Foot UlcersIn an interview with HT Lifestyle, Dr Rajeev Premnath, General Laparoscopic Surgeon and Endoscopist, Minimally Invasive Proctology Department at Ramakrishna Hospital in Bengaluru, shared, "Foot ulcers are chronic open wounds that persistently resist healing or reappear over an extended period. These wounds arise from the breakdown of skin and tissues in the feet and ankles, often leading to infections. Foot ulcers can result from factors like high blood sugar, poor circulation, neuropathy and foot abnormalities."
He cautioned, "Diabetes increases risk due to associated complications. Untreated ulcers can lead to severe complications like infections, abscesses and gangrene, often requiring amputation. Conditions like atherosclerosis and Raynaud's phenomenon also elevate risks. Rarely, ulcers may warrant assessment for skin cancer like squamous cell carcinoma. Foot and ankle ulcers are categorized into three main types: venous ulcers affect lower legs, neurotrophic ulcers occur on diabetic feet, and arterial ulcers due to compromised circulation."
Effects of Circulation and Neuropathy on Foot-Ulcer DevelopmentDr Rajeev Premnath explained, "Diabetes can result in foot ulcers through various mechanisms. Elevated blood sugar levels can induce nerve damage, reducing foot sensation and impairing injury detection. Moreover, diabetes can impede blood circulation, delaying wound healing. Coupled with compromised immune function, even minor injuries or pressure points from improperly fitting shoes can worsen the ulcer."
He added, "Inadequately managed diabetes heightens infection risk, complicating ulcer treatment and potentially leading to severe consequences like gangrene and amputation if neglected. Consistent foot care and effective glucose management are crucial for averting diabetic foot ulcers. Additional health conditions and factors increasing foot ulcer risk include heart and kidney disease, obesity, nerve damage and alcohol and tobacco use."
He suggested the some practical tips for individuals with diabetes to prevent foot ulcers and highlighted that to mitigate the risk of foot ulcers, particularly among individuals susceptible due to conditions like diabetes, adhering to the following guidelines is essential -
Dr Rajeev Premnath said, "Doctors assess foot ulcers, especially in diabetes patients, by visually inspecting the foot, checking for infection, assessing sensation (or lack of it), vascular compromise and assessing blood sugar control and type of footwear used. With adequate circulation and medical care, healing can occur in 3 to 6 weeks, while deeper ulcers may take 12 to 20 weeks, sometimes requiring surgical intervention."
He advised, "Adopting lifestyle modifications to effectively manage diabetes is crucial for promoting foot health. By integrating a balanced diet, regular physical activity and vigilant blood sugar monitoring, survelliance of the foot for injuries/infections early individuals can reduce the risk of complications and enhance overall well-being."
How Stress Can Trigger Ulcer Problems
Ulcers, those gnawing sores in the stomach or duodenum (the first part of the small intestine), often bring visions of greasy food or over-the-counter pain relievers to mind. While these factors can contribute, chronic stress lurks as a significant yet frequently overlooked culprit in ulcer development. This article delves into the connection between stress and ulcers, exploring the biological mechanisms and offering practical tips to manage stress and promote gut health.
Beyond Spicy Food: Unveiling the Roots of UlcersUlcers form when the protective lining of the stomach or duodenum weakens, allowing stomach acid to irritate and erode the tissue. Two main types of ulcers exist:
While these factors are well-established, stress significantly contributes to ulcer development and worsens existing symptoms.
The Gut-Brain Axis: How Stress Fuels Ulcer ProblemsThe gut and brain are intricately connected through a complex network of nerves and hormones called the gut-brain axis. When stress strikes, hormones like cortisol and adrenaline surge through the body. These hormones can increase stomach acid production and weaken the protective lining of the digestive tract, creating an environment ripe for ulcer formation and aggravating existing ones.
Here's a breakdown of how stress can exacerbate ulcers:
While stress may not directly cause ulcers, it undoubtedly plays a significant role. Here are some practical tips for managing stress and promoting gut health:
Ulcers can be painful and disruptive. By understanding the link between stress and ulcers, you can take proactive steps to manage stress and promote gut health. Remember, a healthy mind and a healthy gut work together. If you experience persistent ulcer symptoms, consult your doctor for proper diagnosis and treatment. Early intervention and a holistic approach that addresses physical and emotional well-being are crucial for managing ulcers and achieving optimal gut health.
This story was created using AI technology.
What Is Peptic Ulcer Disease?
Peptic ulcer disease occurs when stomach acid erodes (or destroys) the inner lining of the stomach, causing sores and ulcers inside your stomach. As a result, symptoms like abdominal pain and nausea can develop. If you develop symptoms, it's important to seek care from a healthcare provider soon—as complications like internal bleeding can happen without proper treatment.
There are two main types of peptic ulcer disease—each of which is based on the location of the ulcers. These include: Stomach ulcer: Occurs when the mucous lining in the stomach wall wears away. How deep the erosion of the mucous lining is will often determine the severity of your symptoms. Generally, the deeper the erosion, the more severe the symptoms. Duodenal ulcer: Causes erosion in the duodenum, which is the first and upper portion of your small intestine. Symptoms of a peptic ulcer can vary from person to person. In the early stages, you might not experience any symptoms at all. When symptoms do start, you'll likely experience them during or after eating meals. Common symptoms include: Without proper treatment, peptic ulcer disease can progress and cause bleeding in the stomach wall. If you develop bleeding, the following symptoms may occur: Anemia (low red blood cell levels) Dark stools (poop) Bright red or dark-colored vomit Peptic ulcer disease occurs when the inner lining of the stomach wall erodes. The erosion causes acid to damage the underlying stomach muscles. There are two primary causes of this condition, which include the Helicobacter Pylori (H. Pylori) infection and taking certain medications. H. Pylori is a type of bacteria that triggers an immune system response that inflames and damages the inner lining of the stomach. Because this condition is a bacterial infection, you can develop symptoms by consuming contaminated food and water. Making contact with someone's saliva or other body fluids while they have the infection can also cause you to contract the infection. However, taking certain medications like non-steroidal anti-inflammatory drugs (NSAIDs) can also interfere with the mucous lining of your stomach wall. Many people take NSAIDs to relieve pain symptoms. But long-term use of these medications increases your risk of developing a peptic ulcer. If you are at risk of peptic ulcer disease (such as by having a family history of stomach-related conditions), it's best to ask your healthcare provider about taking NSAIDs before using them. If you experience symptoms of a peptic ulcer, it's important to seek treatment from a healthcare provider as soon as possible to avoid complications from occurring. At your appointment, your healthcare provider will ask about your personal and medical family history—such as which conditions you have, what medications you're taking, and which symptoms you're currently experiencing. They may also ask about your lifestyle habits and dietary choices. Once your provider learns more about your symptoms, they will perform a physical exam to check for signs of a peptic ulcer. To confirm a diagnosis for peptic ulcer disease, your provider will also likely order one or more of the following exams: Upper endoscopy: Uses a special tube that's attached to a small camera that passes through the mouth to look for signs of damage to the mucous lining in the stomach and duodenum. This test is the gold standard way to diagnose peptic ulcer disease. Barium swallow: Involves the use of a special contrast dye while taking an X-ray of the stomach to outline the stomach wall and reveal the presence of any ulcers in the imaging scan. Blood tests: Takes a sample of your blood to check for signs of anemia. H. Pylori tests: Includes breath tests, stool antigen tests, or antibody tests to detect the presence of bacteria. If you receive a diagnosis for peptic ulcer disease, your healthcare provider will recommend medications to improve your symptoms. The goals of treatment are to reduce the production of stomach acid and promote healing of the ulcers. Your healthcare provider will likely prescribe you one of two types of medications: stomach acid inhibitors or H. Pylori medications. Stomach acid inhibitors help stop the production of stomach acid and improve the lining of the stomach wall. For best results, your provider will likely recommend taking these medications about 30 minutes before eating a meal. There are two types of stomach acid inhibitors that your provider may prescribe, which include: Proton pump inhibitors: Prilosec OTC (omeprazole), AcipHex (rabeprazole), or Protonix (pantoprazole) H2-receptor blockers: Zantac (ranitidine) and Tagamet (cimetidine) If the cause of your peptic ulcer is due to an H. Pylori infection, medication will focus on treating the infection. The first-line treatment for H. Pylori infection is a regimen combination, which consists of three antibiotics and a proton pump inhibitor. A common example of a triple medication regimen for H. Pylori is Protonix (pantoprazole), Biaxin (clarithromycin), Moxatag (Amoxicillin), and Flagyl (metronidazole). You'll need to take these medications for one to two weeks to see results. Fortunately, there are several things you can do to reduce your risk of developing a peptic ulcer, such as: Avoid taking NSAIDs without medical supervision Avoid smoking Get screened for H. Pylori infections Engage in stress management activities such as mindfulness, meditation, and exercises. Without proper treatment, peptic ulcer disease can progress and cause the following complications: Upper gastrointestinal bleeding: The most common complication of peptic ulcer diseases and causes internal bleeding in the stomach wall Perforation: Causes holes to develop in the stomach or duodenum, which can lead to an abdominal infection and worsening symptoms without treatment Gastric outlet obstruction: Leads to a blockage in the pylorus (the part of the stomach that connects to the duodenum), making it difficult for food to digest into the small intestine Peptic ulcer disease is a condition that causes sores or ulcers in the stomach when stomach acid destroys the inner lining of the stomach wall. This can happen due to an H. Pylori infection or long-term use of NSAIDs. As a result, symptoms like abdominal pain, bloating, vomiting, and changes in vomit or stool color can occur. It's important to get treatment for peptic ulcers as soon as possible because without treatment, internal bleeding can occur.Thanks for your feedback!


Comments
Post a Comment