Ebola: Symptoms, treatment, and causes
32 Countries With The Highest Rates Of Diabetes
In this article, we will be taking a look at the 32 countries with the highest rates of diabetes. If you do not want to learn about the global diabetes market, head straight to the 5 Countries with the Highest Rates of Diabetes.
The Global Diabetes Market and Its ImplicationsThe global diabetes market is experiencing significant growth and poses a substantial challenge to public health worldwide. According to the IDF Diabetes Atlas, in 2021, approximately 537 million people were suffering from diabetes globally, a number expected to rise to 643 million by 2030 and 783 million by 2045. This increase in prevalence underscores the urgent need for effective measures to address this chronic disease.
In the United States, the diabetes market is substantial, with around 136 million adults diagnosed with diabetes or in a prediabetic condition as reported by the Centers for Disease Control and Prevention. The U.S. Market is dominated by key players such as Abbott, Medtronic, Dexcom, and Insulet Corporation. North America held a significant share of the global diabetes devices market at 38.66% in 2022, driven by a large patient population and favorable reimbursement conditions.
Financially, the global diabetes devices market was estimated at USD 30.31 billion in 2023 and is projected to grow at a compound annual growth rate of 7.45% from 2024 to 2030, reaching USD 32.70 billion. North America led this market in 2022, reflecting the region's high patient numbers and supportive reimbursement environment. Key factors propelling market growth include increasing diabetes incidence, technological advancements in preventive care, and rising demand for blood glucose monitoring devices.
The Diabetic Dilemma: A Global Economic CrisisThe global diabetes epidemic looms large, claiming over 280,000 lives annually. Government initiatives and the development of affordable drugs like oral hypoglycemics are driving market expansion. The toll of diabetes contributes significantly to the global disease burden, estimated at a staggering $16.3 trillion over two decades. Insulin, a lifeline for millions worldwide, experiences soaring demand, particularly in emerging economies. Notably, 94% of insulin pump users reported enhanced quality of life in 2023, fostering robust growth in the insulin pump market, projected to reach $11.4 billion by 2032, growing at an 8.5% CAGR.
Story continues
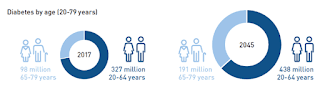
In the United States, insulin costs have surged by over 600% in the last two decades, leading one in four diabetics to ration their supply due to financial constraints. However, investing in affordable options such as biosimilars and generics can alleviate this burden. Major pharmaceutical giants like Sanofi, Eli Lilly and Company, and Novo Nordisk have the potential to mitigate the financial strain on patients and healthcare systems alike. In 2017 alone, diabetes inflicted a staggering 327 billion blow to the US economy, with direct medical expenses totaling $237 billion. Laboratory costs for diabetes management vary widely, ranging from under $5 to over $100 per patient annually.
Sanofi (NASDAQ:SNY), a leading global healthcare company with a century-long legacy, has been instrumental in advancing diabetes treatment and management. Their commitment to developing cutting-edge treatments like TZIELD for Stage 3 type 1 diabetes demonstrates their dedication to enhancing health outcomes. Additionally, their exploration of AI-driven systems for blood glucose analysis reflects a commitment to individualized diabetes support. In Q4 2023, despite a 5% decrease in operating income attributed to various factors, Sanofi (NASDAQ:SNY) experienced significant sales growth, particularly with the anti-inflammatory drug Dupixent. Sanofi (NASDAQ:SNY) anticipates a rebound in adjusted earnings per share in 2025 following a slight decline in 2024. Additionally, Sanofi announced a new chief financial officer, Francois-Xavier Roger, from Nestle, effective April 1, succeeding Jean-Baptiste de Chatillon.
Novo Nordisk A/S (NYSE:NVO), a leading player in the diabetes market, has strengthened its position with a market share increase to 54.9% in 2022. The company dominates the global insulin market with nearly 50% share by volume. Novo Nordisk A/S (NYSE:NVO)'s success lies in innovative products like Ozempic and Wegovy, driving impressive sales growth and enabling it to address unmet needs in type 2 diabetes and obesity.
Anticipating continued growth, Novo Nordisk A/S (NYSE:NVO) expects sales to increase by 18% to 26% this year, fueled by demand for key products. Despite competition, especially in the weight loss segment, the company is confident in meeting market demands through strategic investments.
32 Countries with the Highest Rates of Diabetes
Our MethodologyFor our methodology, we have ranked the countries with the highest rates of diabetes based on age-standardized diabetes rates in these countries in 2021. For the accuracy of data, we relied on IDF Diabetes Atlas.
Here is our list of the 32 countries with the highest rates of diabetes.
32. BangladeshDiabetes Rate: 14.2%
In Bangladesh, diabetes prevalence has surged from 4.5% to 35% between 1994 and 2013. In 2019, 8.4 million adults had diabetes, projected to double by 2045. Prevalence among adults aged 35+ rose from 10.95% in 2011 to 13.75% in 2018, notably among obese individuals. Both genders are affected equally, with prevalence increasing with age.
31. BelizeDiabetes Rate: 14.5%
Belize faces a severe health challenge with a high prevalence of type 2 diabetes (T2D), reaching over 17% in adults, making it the highest in Central and South America and the fifth globally. T2D is now the leading cause of death in Belize, with 33% of the population in the prediabetes range. Diabetes affects both genders, primarily adults aged 20 to 79.
30. TurkeyDiabetes Rate: 14.5%
Turkey has diabetes prevalence of around 14.5% among adults aged 20 to 79, showing an increasing trend from 12.2% in 2014 to 13.2% in 2016. Women represent about three in five cases, with a prevalence of 13.10% compared to 9.12% in men. The diabetes therapeutics market is expected to grow to $2.5 billion by 2030, with Nobel İlaç, Koçak Farma, and GlaxoSmithKline as key players.
29. SyriaDiabetes Rate: 14.9%
Syria stands among the countries with the highest rates of diabetes, totaling 2,918,314 individuals affected. In 2017, adult diabetes cases numbered 705,700, with 12.6% prevalence in females and 11.2% in males. Approximately 400,000 Syrians rely on insulin for survival due to diabetes. Prevalence in Aleppo before 2011 was 14.8% among adults over 25. A cross-sectional survey of Syrian refugees in Jordan found a 5.3% prevalence, with higher rates among those over 60.
28. TongaDiabetes Rate: 15%
In Tonga, 15% of the population faces diabetes, making Tonga stand among the countries with the highest diabetes rates globally. Diabetes predominantly affects adults, especially those aged 41-60. Nearly all Tongans aged 18–69 are at risk for non-communicable diseases, including diabetes.
27. JordanDiabetes Rate: 15.4%
Jordan grapples with a diabetes challenge, with an estimated 866,500 cases in 2021 projected to rise to 1,629,100 by 2045. Diabetes-related health expenditure was USD 849.8 million in 2021, rising to USD 1,234.2 million by 2045, with per capita spending increasing significantly. The most affected age group is 20-79.
26. MicronesiaDiabetes Rate: 15.6%
The Federated States of Micronesia (FSM) stands among the top countries with high rates of diabetes, with a staggering 15.6% prevalence rate as of 2021, attributed to lifestyle changes and a shift to processed foods. Both genders and various age groups are affected. Access to insulin and diabetes treatment is hindered by remoteness, limited healthcare infrastructure, and financial constraints.
25. VanuatuDiabetes Rate: 15.6%
In Vanuatu, diabetes affects 1 in 11 people. Both men and women are impacted. Children are also affected by type 1 diabetes, with 10.9% going undiagnosed, emphasizing the need for early detection and improved healthcare services.
24. Saint Kitts and NevisDiabetes Rate: 16.1%
Saint Kitts and Nevis stand among the countries with the highest rates of diabetes, with a prevalence rate of 16.9%, concentrated in the 45-64 age group, affecting both genders similarly. Comorbidities are prevalent among diabetics, with 76% experiencing additional health issues. By 2045, the North American and Caribbean region, including St. Kitts and Nevis, is projected to have 63 million diabetes cases.
23. United Arab EmiratesDiabetes Rate: 16.4%
The United Arab Emirates (UAE) has a diabetes prevalence rate of 12.3% among adults, totaling around 990,900 cases. In the Northern Emirates, UAE citizens exhibit a 25.1% prevalence. Diabetes prevalence is highest among UAE nationals and Asian non-Arabs, with males at 21% and females at 23%. Healthcare expenditure on diabetes was USD 2,090.4 million in 2021, projected to rise to USD 2,329.3 million by 2030, equating to USD 2,109.5 per person in 2021, and expected to reach USD 2,350.6 per person by 2030.
22. Papua New GuineaDiabetes Rate: 16.7%
Papua New Guinea faces significant diabetes prevalence, with 14.6% of adults affected, totaling approximately 724,000 cases. Even rural areas report high rates, with a village study showing 8.9% diabetes and 5.7% impaired glucose tolerance. Both genders are impacted, with middle-aged individuals, aged 30 to 69, bearing the highest burden of diabetes-related mortality and cases.
21. MexicoDiabetes Rate: 16.9%
Mexico had a diabetes prevalence rate of 16.9% in 2021, impacting around 14 million adults, making Mexico stand among the countries with the highest rates of diabetes. Additionally, 11 million adults have impaired glucose tolerance. Females have a higher risk of diabetes. Diabetes care clinics like Clinicas del Azucar provide affordable care, supported by investments aiming to establish 100 new clinics by 2024.
20. PalauDiabetes Rate: 17%
Palau faces significant diabetes challenges, with 22% of adults diagnosed, totaling 3,015 individuals, and 66% undiagnosed. Financially, insurance contributions and investments totaled $10.5 million in 2023, but medical care payouts were $7.3 million, indicating strain on the system.
19. FijiDiabetes Rate: 17.7%
Fiji stands among the top countries with high rates of diabetes, with prevalence steadily increasing from 16% in 2011 to 17.7% in 2021, projected to reach 20.7% by 2045. The number of diabetes cases is rising, estimated at 99.2 thousand in 2021, and projected to reach 139.7 thousand by 2045. Diabetes affects both genders and various age groups, with a rapid rise attributed to factors like childhood obesity, gestational diabetes, and social transitions, particularly affecting individuals under 60.
18. Saudi ArabiaDiabetes Rate: 18.7%
Saudi Arabia grapples with high diabetes rates, with a prevalence of 17.7% in adults, totaling 4,274,100 cases. Males have a slightly higher prevalence than females, and the highest prevalence is among individuals aged 60 and above. The country faces a significant economic burden due to diabetes, with healthcare expenditure reaching $7,459.5 million in 2021, and a projected national burden exceeding $0.87 billion, excluding indirect costs.
17. SudanDiabetes Rate: 18.9%
Sudan faces with a national diabetes prevalence of 7.7% in adults projected to increase to 10.8% by 2035. Type 2 diabetes mellitus (T2DM) is particularly concerning, with a prevalence of 20.8% in eastern Sudan. Insulin plays a crucial role in treatment, especially for youth with T2DM, alongside medications like metformin, glibenclamide, glimepiride, and glipizide.
16. MalaysiaDiabetes Rate: 19%
In Malaysia, approximately 18.3% of adults were affected by diabetes, according to the National Diabetes Registry Report. The prevalence has steadily increased from 13.4% in 2015 to 18.3% in 2019. Elderly individuals, especially those aged 60 and above, bear the highest burden, with rates reaching 33.46%. Ethnic disparities exist, with Indians having the highest prevalence at 25.10%. Despite a high treatment rate of 87.5%, only 21.8% of treated individuals have their diabetes under control, indicating a need for improved management strategies.
15. GuamDiabetes Rate: 19.1%
Guam had a diabetes prevalence rate of 19.1% in 2021, up from 13.7% in 2018. Approximately one in six residents is affected, with the indigenous Chamorro population experiencing higher rates. Individuals aged 45 and older are at higher risk, raising concerns due to Guam's relatively young population.
14. QatarDiabetes Rate: 19.5%
Qatar faces a significant challenge with diabetes, with a prevalence of around 19.5%, expected to rise to 24% by 2050, making Qatar stand among the top countries with high rates of diabetes. The SMART clinic provides tailored care plans, emphasizing blood glucose, pressure, and lipid levels.
13. Solomon IslandsDiabetes Rate: 19.8%
The Solomon Islands had a diabetes prevalence rate of 19.8% in 2021. Both genders and various age groups are affected, with adults aged 30 to 69 being the most impacted. Despite the high prevalence, insulin usage remains low at approximately 6%, indicating a need for improved management strategies.
12. TuvaluDiabetes Rate: 20.3%
Tuvalu, a Pacific island nation, had a diabetes prevalence rate of 20.3%. Females have a slightly higher prevalence at 23.8% compared to males at 22.4%. The remote location and scarce healthcare facilities hinder access to essential treatments, including insulin, exacerbating the challenge of controlling the disease.
11. American SamoaDiabetes Rate: 20.3%
American Samoa faces one of the world's highest rates of diabetes, particularly among adults aged 20 to 79. The prevalence of Type 2 diabetes mellitus has been steadily increasing over the years, with projections indicating further escalation. Adults aged 25 to 64 have witnessed a significant rise in Type 2 diabetes prevalence, highlighting a growing health challenge in this age group.
10. EgyptDiabetes Rate: 20.9%
Egypt faces a significant challenge with diabetes, with a prevalence rate of approximately 15.2% among adults. The number of adult diabetic patients was around 8,850,400 in early 2020 and is expected to rise significantly by 2035. Type 2 diabetes prevalence is approximately 15.6% among adults aged 20 to 79.
9. KiribatiDiabetes Rate: 22.1%
Kiribati stands ninth among the countries with the highest rates of diabetes, with over 20% of adults affected by type 2 diabetes. Both genders and various age groups are impacted, including children with type 1 diabetes, highlighting gaps in healthcare awareness. Access to insulin is crucial for type 1 diabetes management, with early diagnosis being essential to prevent fatal consequences.
8. MauritiusDiabetes Rate: 22.6%
Mauritius had a a diabetes prevalence rate of 26.5% among adults, totaling 250,400 cases. Both men and women have seen a substantial increase in diabetes prevalence over the years, with a 64% rise since 1987. The most affected age group is adults aged 20 to 79 years.
7. Marshall IslandsDiabetes Rate: 23%
The Republic of the Marshall Islands (RMI) is one of the countries with the highest global prevalence of diabetes. By 2045, the estimated number of diabetes cases is expected to rise from 9.1 thousand to 13.1 thousand, with an increase in prevalence from 23.0% to 26.0%. Diabetes-related health expenditure was USD 13.6 million in 2021, projected to reach USD 18.1 million by 2045, emphasizing its economic impact on healthcare spending.
6. NauruDiabetes Rate: 23.4%
Nauru stands sixth among the countries with the highest rates of diabetes, affecting both men and women. The prevalence of diabetes was reported at 23.4% in 2021, with risk factors including age, high cholesterol levels, and waist circumference. Older adults, especially those aged 55-64 years, are most vulnerable. The financial burden on the Nauru government due to diabetes was estimated at AUD12.8 million in 2017, emphasizing the need for effective management strategies.
Click to see and continue reading the 5 Countries with the Highest Rates of Diabetes.
Suggested Articles:
Disclosure. None: The 32 Countries with the Highest Rates of Diabetes is originally published on Insider Monkey.
If A Diabetes Policy Of Diet And Exercise Keeps Failing, Is It Time For A New Approach?
Fifty years ago, a diabetes survey in the Republic of Nauru concluded that a third of Nauruans had type 2 diabetes. It was the first time the relatively uncommon disease was found to be widespread in a national population, and it led researchers to raise the alarm about a potential "global diabetes epidemic".
At the time, there was little other research about population-scale diabetes, so the researchers made some assumptions to explain their data and propose a way forward. First, they said that diabetes in Nauru was probably caused by a genetic predisposition of islander populations to diabetes (a hypothesis later critiqued by its original author, and which remains unsupported by data – archaeological, anthropological or genetic); modernisation of islander lifestyles leading to a high-calorie diet (a theory my colleagues and I have since challenged); and reduced physical activity, and obesity. Second, they suggested these causes could be best addressed by nutrition and lifestyle education.
Subsequent surveys have built on these assertions, and for 50 years researchers have focused predominantly on diet and physical activity as both cause and cure for type 2 diabetes in Nauru.
Despite decades of interventions informed by these surveys, type 2 diabetes remains a leading cause of death and disability, along with heart disease and stroke, in the Pacific island nation. There is also significant diabetes-related disability, from gangrenous or amputated limbs to blindness to kidney disease, and many people experience debilitating side-effects of diabetes medications. Life expectancy remains low: about 60 years for men and 66 for women.
Quick Guide A common condition ShowThe human toll of non-communicable diseases (NCDs) is huge and rising. These illnesses end the lives of approximately 41 million of the 56 million people who die every year – and three quarters of them are in the developing world.
NCDs are simply that; unlike, say, a virus, you can't catch them. Instead, they are caused by a combination of genetic, physiological, environmental and behavioural factors. The main types are cancers, chronic respiratory illnesses, diabetes and cardiovascular disease – heart attacks and stroke. Approximately 80% are preventable, and all are on the rise, spreading inexorably around the world as ageing populations and lifestyles pushed by economic growth and urbanisation make being unhealthy a global phenomenon.
NCDs, once seen as illnesses of the wealthy, now have a grip on the poor. Disease, disability and death are perfectly designed to create and widen inequality – and being poor makes it less likely you will be diagnosed accurately or treated.
Investment in tackling these common and chronic conditions that kill 71% of us is incredibly low, while the cost to families, economies and communities is staggeringly high.
In low-income countries NCDs – typically slow and debilitating illnesses – are seeing a fraction of the money needed being invested or donated. Attention remains focused on the threats from communicable diseases, yet cancer death rates have long sped past the death toll from malaria, TB and HIV/Aids combined.
'A common condition' is a Guardian series reporting on NCDs in the developing world: their prevalence, the solutions, the causes and consequences, telling the stories of people living with these illnesses.
Tracy McVeigh, editor
Was this helpful?
Thank you for your feedback.
How is it possible that 50 years later, when evidence points to little improvement, we are still making similar assumptions and coming to similar conclusions about type 2 diabetes?
What if the assumptions were wrong?In the early 2010s, I set out to study obesity in Nauru. Building on previous research, I aimed to trace how people's diets and physical activity had changed throughout the 20th century. Yet during my year on the island, it became clear that diet and activity were not the most significant changes the people of Nauru felt they had experienced.
I had assumed that decades of diabetes research on the island must be right. Now, I'm not so sure
I pivoted my research to focus on their voices. I documented histories of low socioeconomic status, social stress and fraying families linked to colonialism, wealth, poverty and land loss on the island. I learned about changes linked to globalisation, medicine, mining, technology, migration and two world wars. I avoided drinking from the national desalination plant, which often had high levels of bacteria. I inhaled the fog of fine white dust from the phosphate mines that left a powdery film of "Nauruan snow" through houses and on my glasses.
These aspects of Nauruan life all coincide with the rise of type 2 diabetes as a population-wide phenomenon on the island. They do not, however, fit neatly into the 50-year-old framing of diabetes as simply a product of individual diet and physical activity behaviours.
I had initially assumed that the medical facts that echoed through the decades of diabetes research on the island must be right, and that my social research was somehow flawed. Now, I'm not so sure. A creeping sense of doubt has led me to pause and question the assertions made in that initial diabetes survey.
Debunking the idea of an isolated nationIn 1974, just six years after Nauru gained political independence from colonial powers, the Nauruan minister for health and education, Austin Bernicke, gave the go-ahead for the world's first national diabetes survey.
The Australian survey team tested 100 people on the first day. The results were so unexpected that one of the researchers assumed the blood glucose methodology was flawed and promptly returned to Melbourne.
Yet the methodology was sound. The survey concluded that 34% of Nauruans – and two-thirds of those aged over 40 – had diabetes.
The final report's suggestion that western diets and activity levels had led to diabetes among islanders – but not among westerners – hinged on a third assumption: that islands such as Nauru had been isolated from "contact with white men" until the second world war, after which rapid modernisation occurred.
Evidence paints a different picture. Since the late-1800s, the people of Nauru had different facets of life controlled by different colonial authorities (including Germany, Britain, New Zealand and Australia). They had experienced racial segregation, Japanese occupation, and a fight for political independence. They had been subjected to education programmes in missions and colonial schools and engaged with the cultures of whalers, traders and Chinese mining labourers. With its commercial and strategic significance as a wireless and telegraphy station, and its high-grade phosphate used to fertilise crops in many nations, Nauru has been connected to the world for more than a century longer than the report had assumed.
skip past newsletter promotionSign up to Global Dispatch
Get a different world view with a roundup of the best news, features and pictures, curated by our global development team
Privacy Notice: Newsletters may contain info about charities, online ads, and content funded by outside parties. For more information see our Privacy Policy. We use Google reCaptcha to protect our website and the Google Privacy Policy and Terms of Service apply.after newsletter promotion
The survey team did not look at this history, perhaps because they had already narrowed their scope to focus on factors that had previously been linked to diabetes in individuals. They recommended that the Nauru government should change diet and physical activity levels in the nation by appointing an overseas-trained dietician, and importing western diet and exercise education.
Considering factors beyond diet and exerciseOur continued emphasis on intervening in diet and physical activity to address diabetes in Nauru is curious given that some research in the past 50 years has pointed to other possibilities. For example, low socioeconomic status, chronic stress, social isolation and loneliness and systemic inflammation have all been linked to diabetes, as well as exposure to poor air quality and changing gut microbiota.
We find these in Nauru – if we look for them. Yet such possibilities never seem to find a way into shaping interventions, medical education or government decision-making. This extends well beyond diabetes in Nauru. The global mantra of type 2 diabetes continues to centre on diet and exercise, and sometimes genetics, with little accommodation for other contributing factors. For example, the World Health Organization's fact sheet on diabetes states: "Factors that contribute to developing type 2 diabetes include being overweight, not getting enough exercise, and genetics."
Air pollution raises risk of type 2 diabetes, says landmark Indian study
Read more
We don't often talk about it, but a significant barrier to improving public health outcomes is identifying when a belief assumed to be "fact" no longer serves us, such as the belief that cholera was caused by bad air. It can take decades for such beliefs to harden as "fact" among medical practitioners, decision-makers and the public, and decades more to chip them away again. Perhaps diabetes is no different.
Finding new ways forwardIf a starting assumption about health is flawed, then any new intervention, however innovative, will at best fail, and at worst aggravate the problem. By doubting historical assertions about diabetes, by re-examining what we believe to be "fact", and why, we create space for new questions, perspectives and possibilities for intervention. For example, what are the links between colonialism, land loss, socioeconomic inequality, chronic stress and diabetes on the island? How have islanders' microbiome and mycobiome changed over time and what are the population health implications? Could we consider diabetes as a product of population exposures to inflammatory agents, from ultra-processed foods to poor air, and intervene by holding to account those responsible for such exposures?
This does not necessarily preclude diet or physical activity as contributory factors, but it does require us to ask more questions about why these factors have come to dominate the type 2 diabetes landscape, where they might fit in future, what are the unintended consequences of intervening in them, and how to de-centre something so tightly held as a universal truth.
If we let go of 50-year-old ways of thinking, places such as Nauru may help the rest of the world to find new ways forward.
Amy McLennan is a senior fellow at the School of Cybernetics at the Australian National University and a research affiliate at the School of Anthropology, University of Oxford, UK
Revolutionizing Weight Loss: Scientists Uncover New Secrets To Natural Appetite Control

A new study unveils that Metformin and solid foods raise a natural appetite suppressant, Lac-Phe, offering promising strategies against obesity and type-2 diabetes. This insight into Metformin's role and the impact of food choices on hunger control opens avenues for novel anti-obesity treatments and dietary guidelines.
In a ground-breaking study, just published in leading international journal Nature Metabolism, scientists from Trinity College Dublin and Princeton and Harvard Medical School share newly uncovered secrets to natural appetite control, which offers promise in the battle against obesity and type-2 diabetes.
The new research shows the diabetes drug Metformin and solid foods elevate a hunger-reducing factor (Lac-Phe) in the body, while sugary drinks have minimal effects.
Obesity is a key driver of type-2 diabetes, and the 2022 Eurostat report revealed that 1 in 5 Irish adults are obese. Indeed, global diabetes cases have more than tripled in the last 20 years alongside the rise in obesity. The cost of managing diabetes represents approximately 9% of EU Member States' healthcare budgets – totaling €149 billion in 2019.
There is no cure for diabetes and every year in Europe 114,000 people lose their lives from diabetes-related complications.
Metformin's Role in Appetite SuppressionThe scientists now report new insights into how the widely used diabetes drug metformin benefits patients with type-2 diabetes. Metformin is described by some as a "wonder drug" even though we still do not know exactly how it works.
This study shows that metformin increases the amount of an appetite-suppressing factor called Lactoyl-Phenylalanine (Lac-Phe), identified in 2022 as a natural appetite suppressant, and which is known to be raised by vigorous exercise.
The scientists probed data from other studies involving large numbers of patients, to conclusively demonstrate that Lac-Phe levels rise after individuals take metformin. This work opens a new avenue for developing targeted anti-obesity treatments.
Insights from ResearchersBarry Scott, first author of the research, is a former stock market trader and now a Ph.D. Candidate in Trinity's School of Biochemistry and Immunology, based in the Trinity Biomedical Sciences Institute (TBSI). He said: "I'm hopeful our research can have a big impact. Metformin is the most prescribed drug for type-2 diabetes, and it's very safe and well-tolerated. How metformin affects appetite was not known, but this work shows that its influence on Lac-Phe is a key part of its hunger-suppressing impact."
The team also discovered that Lac-Phe increases after eating, and so contributes to the feeling of fullness after a meal.
David Finlay, Associate Professor in Immunometabolism, Trinity, who co-supervised the work with Professor Lydia Lynch, Princeton and Harvard Medical Schools, said: "Our study shows that the type of food you eat matters. For instance, eating sugar-rich date fruits caused an immediate and large surge in Lac-Phe, for example, whereas drinking a sugar-rich drink did not. This could help explain why liquid calories can drive obesity."
Professor Lydia Lynch said: "Identifying the factors that control appetite and satiety after a meal is important to help us to understand and ultimately treat the current obesity epidemic. Further understanding Lac-Phe's actions may lead to a new class of safe and effective anti-obesity drugs."
Reference: "Metformin and feeding increase levels of the appetite-suppressing metabolite Lac-Phe in humans" by Barry Scott, Emily A. Day, Katie L. O'Brien, John Scanlan, Grace Cromwell, Aine Ni Scannail, Marie E. McDonnell, David K. Finlay and Lydia Lynch, 18 March 2024, Nature Metabolism.DOI: 10.1038/s42255-024-01018-7
The study was funded by the National Institutes of Health and the Science Foundation Ireland.



Comments
Post a Comment