New Vaccines in the Pipeline 2020
Doctors Share Warning Signs After Virginia College Athlete Sidelined By Heart Condition
A University of Virginia athlete was recently diagnosed with a heart condition that pose a serious risk to young athletes -- but it can also be difficult to detect. Here are the warning signs doctors say you should never ignore.
Tucker Mullen played lacrosse at UVA — until last fall, when he was sidelined with chest pain during practice.
"It felt like someone had a light hand kind of pushing on my chest," Mullen said. "Eventually during one of the practices, it was too much and I was unable to breathe well and got shortness of breath very, very quickly."
Doctors ran a series of tests, but everything came up normal. However, his symptoms didn't go away.
"And that's what the scariest thing was," said his mom, Lisa Mullen. "His chest pressure, nothing would help it. So it was the unknown, like, what is wrong? They kept ruling out this — 'It's not this;' 'It's not that;' 'His heart looks good; he's healthy' — and I'm like, 'OK, but why does he feel like this?'"
She was still worried, especially after hearing stories of young athletes such as Damar Hamlin and Bronny James suffering cardiac arrest while playing sports at a competitive level. That's when they went to Children's National Hospital in D.C. For a second opinion. Doctors there did another round of screenings, including a stress test, as well as a cardiac MRI that uncovered the issue.
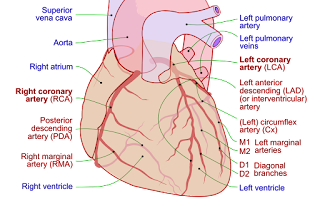
Tucker Mullen had a congenital heart condition called anomalous origin of the right coronary artery, in which where one of the coronary arteries that brings blood to the body was routed around his heart in a way that restricted blood flow, which could lead to a heart attack.
U.S. & WorldNews from around the country and around the globe
It's the second leading cause of sudden death among athletes.
"Screening is not so easy to detect this, as you saw from Tucker's case," said Dr. Charlie Berul, a cardiologist at Children's National Hospital who treated Mullen. "He had an evaluation even after symptoms, and the initial evaluation was thought to be normal."
Berul says most people don't even know they have this condition and can live a normal, healthy life without having symptoms or needing surgery. But there are warning signs to look out for, especially for athletes.
"We worry more and raise a red flag if there's exertion symptoms," Berul said. "Chest pain with exercise or fainting with exercise is a lot more concerning than fainting when you stand up too fast or a sharp chest pain because you tweaked a muscle in your chest wall, which is so common in teenagers."
At 21, Mullen had open heart surgery the day before Thanksgiving.
Now he's on the mend, thankful to be treated before suffering any serious complications on the field. Doctors say they're amazed at his progress as he gears up for his comeback while encouraging other athletes to speak up when something doesn't feel right.
"It's OK to ask for help, and it's OK to feel like something is off," Mullen said. "I think a lot of the times, people are afraid to speak up because they don't want to miss time or lose a spot. In my case, if I didn't speak up about it, I could have had some really scary effects down the line."
Mullen's story is a reminder for parents and athletes to be mindful of their bodies and proactive about their health. Doctors say this particular heart condition occurs three times more often in men than women, although the reason why isn't entirely clear. If you have concerns, you can reach out to your child's primary care physician or pediatrician.
Why I'm Running: 'Without Their Diligence I Would Not Have Survived'
Readers SayIn our "Why I'm Running" series, Boston Marathon runners share what's inspiring them to make the 26.2-mile trek from Hopkinton to Boston. If you're running the marathon, you can share your story here.
Name: Diana WoodAge: 41From: Norwell
I am running the marathon to support Boston Children's Hospital. The doctors at Children's saved my life as a child and are currently treating my dear friend's son, Cam Robinson.
Cam suffers from homozygous familial hypercholesterolemia (HoFH), a rare life-threatening genetic condition that causes accelerated cardiovascular disease and puts him at risk of a fatal cardiac event. He was diagnosed at age 5. A cardiologist ran his cholesterol levels and his LDL was 897 (well above the healthy target of below 120) and he already had a 90% blockage in his right coronary artery. He needed immediate treatment. At that time, the only options were a 6-hour weekly treatment called LDL apheresis or a liver transplant. Cam had a port placed in his chest at the age of 5 and has endured 275 treatments to date.
The care he has received has been life-changing for their family. Without them, Cam would not be where he is today. Like Cam, I was diagnosed with a rare condition calm transient erythroblastopenia of childhood (TEC), which is a form of anemia that can be fatal because of its benign symptoms. Children's identified the conditions after other doctors missed it. After several blood transfusions I made a full recovery, but without their diligence I would not have survived. Now as a mother myself, I wanted to run to support such an amazing organization who is helping Cam, helped me and will continue to help countless children in the years to come.
Editor's note: This entry may have been lightly edited for clarity or grammar.
Sign up for the latest Boston Marathon updates👟 Everything you need to know about Marathon Monday, delivered to your inbox.
Intravascular Imaging Lowers Risk Of MACE At 1 Year In Left Main PCI
IVUS image after PCI for a bifurcation LM lesion showing the minimal stent area and the maximal stent diameter. Photo Credit: Ahmed Bendary
Use of intravascular imaging with IVUS to guide revascularization of unprotected left main coronary artery lesions significantly improves clinical outcomes when compared with conventional PCI, according to results of a new randomized, controlled study.
At 12 months, the rate of major adverse cardiovascular events was 3.3% among the IVUS-treated patients versus 18.7% in the conventional PCI study arm (P < 0.001), a difference that was driven by a lower rate of target vessel revascularization, investigators reported recently in the journal Coronary Artery Disease.
"The advantages of using IVUS or OCT for interventions in the left main coronary artery are clear," lead investigator Ahmed Bendary, MD (Benha University, Egypt), told TCTMD. "They offer us an unparalleled view inside the artery, helping to assess the lesion's severity, ensure proper stent sizing, and verify stent expansion and apposition postdeployment. This leads to better procedural outcomes and a significant reduction in MACE rates. Essentially, these tools allow us to 'measure twice, cut once,' ensuring the highest level of precision in these critical interventions."
Bendary said that while their study—which used IVUS alone, not optical coherence tomography (OCT)—was on the smaller side, the results are both promising and significant. "It adds to the growing body of evidence supporting the broader use of intravascular imaging," he said. "While a larger study could provide more data and potentially sway the consensus further, our findings already make a strong case for considering IVUS as a standard part of the toolkit for left-main revascularization."
Ajay Kirtane, MD (NewYork-Presbyterian/Columbia University Irving Medical Center, New York, NY), a member of the American College of Cardiology (ACC) Interventional Council, commended the investigators for performing this single-center randomized trial but noted the effect sizes seen were larger than what would normally be expected. It is possible, he said, to achieve very good outcomes with an angiography-guided approach with operators who adhere to good procedural techniques, such as adequately sizing the stent and use of postdilatation.
However, even when adhering to best practices, operators won't always achieve the same outcomes as when using IVUS, said Kirtane. Moreover, the data consistently show that when compared head-to-head against the standard of CABG surgery in left main coronary disease, PCI is associated with higher rates of repeat revascularization.
"I'm a strong believer that if you're going to stent the left main—especially because our comparator group is surgery—we need to do everything we can to lower the rates of repeat revascularization," Kirtane told TCTMD. "Imaging is one of those components. I strongly believe you should do it routinely, and I do think these data are supportive of that."
Although IVUS was not mandated in either EXCEL or NOBLE, it was strongly recommended per the study protocols and was used in roughly 75% of PCIs. "It's hard to say we're not going to do imaging because in the trials that studied [PCI in left main CAD], it was used," he said.
Last year, the ACC Interventional Council published a review advocating for the routine use of intravascular imaging during PCI. These imaging tools, which include IVUS, OCT, and near-infrared spectroscopy (NIRS), are an essential adjunct to angiography for certain lesion subsets, including those in the left main coronary artery, according to the experts.
Studies presented and published last year also largely support the routine use of IVUS or OCT, with all showing that these imaging tools led to better stent implantation, fewer complications, and less stent thrombosis. In RENOVATE COMPLEX-PCI and OCTOBER, intravascular imaging lowered the risk of target vessel failure and MACE, respectively. While ILUMIEN IV, a study of 2,500 high-risk patients with high-risk lesions, failed to show any difference in target lesion failure with OCT, an updated meta-analysis did show that IVUS/OCT was superior to angiography alone for reducing of cardiac death, MI, and target lesion revascularization.
Randomized to IVUS or Angiography Alone
In this new study, investigators randomized 210 patients (mean age 62 years; 71.3% male) with left main coronary artery disease to PCI with IVUS or the control group without IVUS assessment. The lesion in the left main artery was located in the distal, midshaft, and ostial regions in 76.8%, 13.8%, and 9.4% of patients, respectively. Approximately 80% of patients had a SYNTAX score of 32 or less. There was no significant difference in baseline or lesion characteristics between study groups.
There was greater use of predilatation before stenting in the IVUS group than in the control group. Additionally, postdilatation balloon diameters, stent diameters, pressure for postdilatation, and procedural costs were all higher in the IVUS arm.
The risk of MACE—a composite of MI, target vessel revascularization, cardiac death, and stent thrombosis—was significantly lower in the IVUS arm at 12 months. In the angiography-alone group, there were two deaths, three MIs, 10 target vessel revascularizations, and two stent thromboses versus three cases of target vessel revascularization in the IVUS group. In the Kaplan-Meier analysis, the use of IVUS was associated with an 84.4% lower risk of MACE at 1 year after controlling for age, body mass index, gender, and other risk factors.
Bendary likened use of intravascular imaging for stent placement to getting a tailored suit. "It's not just about getting a stent in place," he said. "It's about ensuring the stent fits just right." Such imaging, he said, provide "a closer, more detailed look at the artery, something traditional angiography can't match."
There are some concerns about the use of IVUS in the left main coronary artery, primarily related to the potential for arterial injury or disruption of atherosclerotic plaque. "However, in skilled hands, these risks are minimal compared to the benefits," said Bendary. "These tools give us a live view of what's happening inside the arteries, allowing for precise stent placement and optimal expansion, which is crucial in the left main due to its significant myocardial territory."
Bendary added that the guidelines are beginning to reflect the growing body of evidence in support of intravascular imaging. The ACC, American Heart Association, and the Society for Cardiovascular Angiography and Interventions guidelines for coronary revascularization recommend IVUS for procedural guidance, particularly in left main or complex CAD (OCT is specified as a reasonable alternative to IVUS for procedural guidance, except in ostial left main disease). Guidelines from the European Society of Cardiology and European Association for Cardio-Thoracic Surgery also recommend IVUS or OCT for selected patients to optimize stent implantation.
In the US guidelines, surgery is a class 1a recommendation for stable patients with significant left main stenosis while PCI is a class 2a indication for those with low-to-medium anatomical complexity. In Europe, guidelines are a little in flux following years of disagreements around various clinical trials, most notably EXCEL. Currently, both PCI and CABG are class 1a recommendations for patients with left main CAD and a low SYNTAX score, but a recent task force suggested that PCI should be downgraded to a class 2a recommendation for stable patients with left main disease and a low-to-intermediate anatomical complexity.



Comments
Post a Comment