Treating Zaire ebolavirus With Ansuvimab-zykl - Contagionlive.com
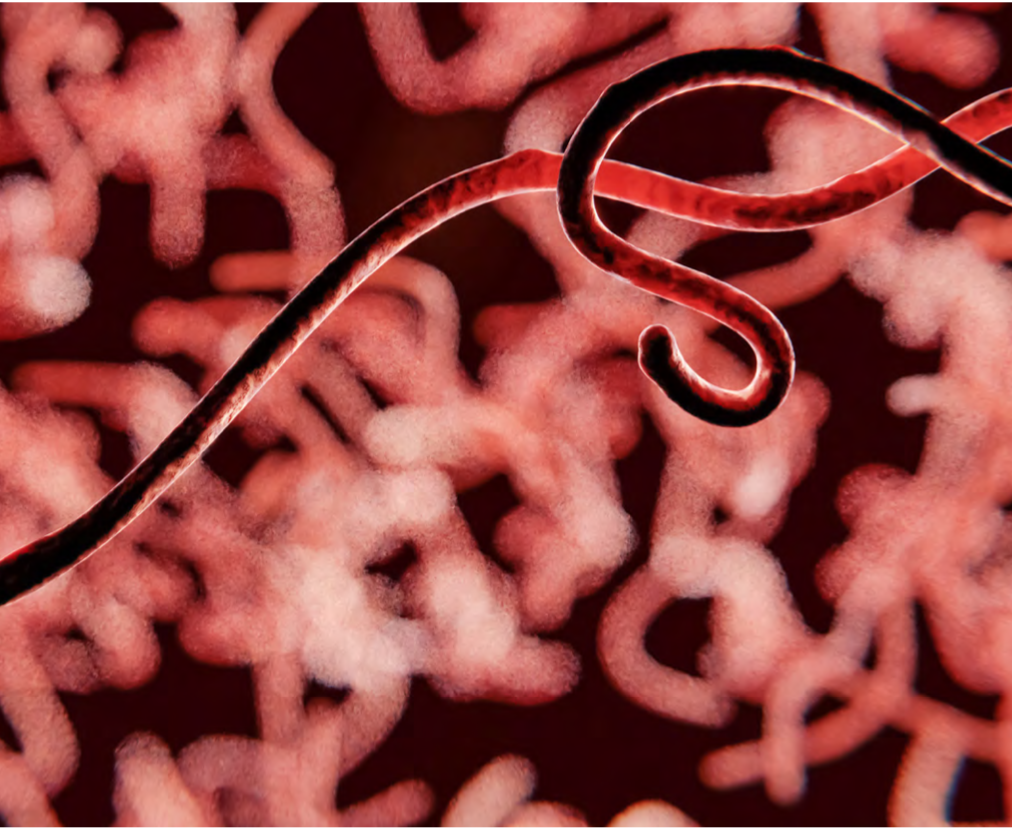
Zaire ebolavirus (EBOV)is 1 of 4 Ebolavirus species that can cause a potentially fatal disease in humans.1 The Ebola virus is thought to be introduced into humans through contact with blood, bodily secretions, or organs of infected animals, such as bats, apes, monkeys, antelope, or porcupines.2 Human-to-human transmission occurs through direct contact with blood, bodily fluids, and tissues of infected humans as well as contaminated surfaces and materials.1
The 2014-2016 Ebola outbreak was the largest recorded, with a total of 28,652 cases reported in 10 countries and 11,325 deaths occurring in 6 of those countries.3,4 The World Bank reported that the outbreak cost an estimated $1.62 billion.5
Spurred by this outbreak, the World Health Organization initiated discussions to develop and utilize experimental therapeutics in the next Ebola outbreak.3 Development of ansuvimab-zykl (Ebanga) originated from a single monoclonal antibody isolated from immortalized B cells obtained from a survivor of the 1995 Ebola outbreak in the city of Kikwit in the Democratic Republic of the Congo.6 Ansuvimab-zykl is a single-dose, intravenous, recombinant human IgG1k monoclonal antibody that binds to the glycoprotein 1 subunit of EBOV, preventing binding of EBOV to host cells and inhibiting viral entry into the host cell.7
A phase I, open-label, dose-escalation clinical trial for ansuvimab-zykl was conducted from March 2018 to September 2018 to evaluate its safety, tolerability, and pharmacokinetics.8 The trial included 18 subjects in 3 experimental arms (5 mg/kg, n=3; 25 mg/kg, n=5; and 50 mg/kg, n=10), with the drug given as a single 30-minute infusion. Participants were followed for 24 weeks and assessed for infusion-site reactions and systemic symptoms through self-reporting, direct clinician assessment, and clinical laboratory data. The primary study outcome was safety and tolerability of ansuvimab-zykl; secondary outcomes included pharmacokinetic and antidrug antibody evaluation.
All doses were well tolerated, with no infusion-site reactions reported. Only 4 (22%) participants experienced systemic symptoms, including malaise (n=3), myalgia (n=2), headache (n=4), chills (n=2), nausea (n=2), and joint pain (n=2). There were no serious adverse events. Ansuvimab-zykl exhibited linear pharmacokinetics and had a half-life of 24 days, with no detection of antidrug antibodies noted.
When the next EBOV outbreak occurred in August 2018,9 the randomized, controlled PALM trial (NCT03719586) was initiated comparing MAb114 (now ansuvimab-zykl), remdesivir, and REGN-EB3 to ZMapp (active control).3 Patients were enrolled from November 2018 through August 2019, and all were included if they had a positive reverse transcriptase–polymerase chain reaction (RT-PCR) assay positive for EBOV within 3 days prior to screening. The primary end point was death at 28 days, and the secondary efficacy end point was time to first negative PCR test.
Most patients (74.4%) enrolled were 18 years or older, and more than half (55.6%) identified as female (Table).3 A total of 673 participants were randomized as follows: 169 received ZMapp (50 mg/kg×3 doses); 175 received remdesivir (200 mg×1 dose, then 100 mg daily×9-13 days); 174 received MAb114 (50 mg/kg×1 dose); and 155 received REGN-EB3 (150 mg/kg×1 dose). Twelve patients died prior to receiving the first dose: 1 in the ZMapp group, 3 in the remdesivir group, 3 in the MAb114 group, and 5 in the REGN-EB3 group.
Most participants received the study drugs within 6 hours of enrollment in the trial; however, 42 (6.2%) patients had therapy delayed for more than 6 hours. Participants in the ZMapp group received the drug in just over 3 hours, and participants in the MAb114 group received the drug in just over 2.5 hours. Twenty-nine participants experienced a serious adverse event related to the trial drugs: 7 who received ZMapp, 9 who received remdesivir, 10 who received MAb114, and 3 who received REGN-EB3.
By day 28, 290 (43.1%) patients expired; however, MAb114 had significantly less deaths compared to ZMapp (35.1% vs 49.7%; 95% CI, –25.2 to –1.7). This result continued to hold true for patients of both high (69.9% vs 84.5%; 95% CI, –33.0 to –0.5) and low (9.9% vs 24.5%; 95% CI, –32.4 to –2.6) viral loads, as well as for those who received the drugs in less than 6 hours (34.5% vs 49%; 95% CI, –25.4 to –1.5).
When examining the impact of other variables through a logistic regression model for death at 28 days, MAb114 maintained superiority over ZMapp when considering duration of EBOV symptoms (odds ratio [OR], 0.49; 95% CI, 0.31-0.78), age (OR, 0.52; 95% CI, 0.33-0.82), and serum creatinine level (OR, 0.48; 95% CI, 0.27-0.84). Additionally, the secondary efficacy end point, median time to first negative PCR test, was shorter for patients receiving MAb114 than patients receiving ZMapp (16 days vs 27 days).3
Ansuvimab-zykl was formally approved by the FDA on December 22, 2020, for the treatment of infection caused by Zaire ebolavirus in adult and pediatric patients, including neonates born to a mother who is PCR positive for Zaire ebolavirus.7 See Figure10 for the development timeline of ansuvimab-zykl. The drug is recommended to be given as a single 50 mg/kg actual body weight dose infused through a 1.2 micron in-line filter extension set over 60 minutes.7
No studies have been done to determine the impact of infusion ansuvimab-zykl in a patient who has received or will receive the live Ebola vaccine; therefore, it is recommended to avoid concurrent administration of the vaccine with ansuvimab-zykl treatment. Ansuvimab-zykl is approved for use in special populations, including pregnant women and neonates. Although an insufficient number of patients older than 65 years were included in the PALM trial, there were no differences in responses compared to adults younger than 65 years.
With the current outbreaks of EVOD occurring in the Democratic Republic of the Congo and Guinea, patients of any age can receive ansuvimab-zykl to help increase their chances of survival.2 The only limitation to using this drug is the need to store product vials in a refrigerated condition prior to warming and reconstitution.7
Lauren Black, PharmD candidate, is a fourth-year student pharmacist at the University of Mississippi School of Pharmacy.
Matthew Wittman, PharmD candidate, is a fourth-year student pharmacist at the University of Mississippi School of Pharmacy.
Jamie Wagner, PharmD, BCPS, is a clinical assistant professor at the University of Mississippi School of Pharmacy and an antimicrobial stewardship pharmacist at St Dominic Hospital in Jackson. She is immediate past chair of the Society of Infectious Diseases Pharmacists (SIDP)Antimicrobial Stewardship Committee, a member of the SIDP Strategic Planning Committee, and a member of the American College of Clinical Pharmacy ID PRN Research Committee.
References
- FDA approves treatment for Ebola virus. FDA. Updated December 21, 2020. Accessed April 29, 2021. https://www.fda.gov/drugs/drug-safety-and-availability/fda-approves-treatment-ebola-virus
- Ebola virus disease. World Health Organization. February 23, 2021. Accessed April 29, 2021. https://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease
- Mulangu S, Dodd LE, Davey RT Jr, et al.; PALM Consortium Study Team. A randomized, controlled trial of Ebola virus disease therapeutics. N Engl J Med. 2019;381(24):2293-2303. doi:10.1056/NEJMoa1910993
- 2014-2016 Ebola outbreak in West Africa. CDC. Updated March 8, 2019. Accessed April 29, 2021. https://www.cdc.gov/vhf/ebola/history/2014-2016-outbreak/index.html
- Wojda TR, Valenza PL, Cornejo K, et al. The Ebola outbreak of 2015-2015: from coordinated multilateral action to effective disease containment, vaccine development, and beyond. J Glob Infect Dis. 2015;7(4):127-138. doi:10.4103/0974-777X.170495
- Ridgeback Biotherapeutics LP announces the approval of Ebanga for Ebola. News release. Ridgeback Biotherapeutics LP. December 22, 2020. Accessed April 29, 2021. https://www.businesswire.com/news/home/20201222005421/en/Ridgeback-Biotherapeutics-LP-Announces-the-Approval-of-EbangaTM-for-Ebola
- Ebanga. Prescribing information. Ridgeback Biotherapeutics LP; 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/761172s000lbl.pdf
- Gaudinski MR, Coates EE, Novik L, et al; VRC 608 Study team. Safety, tolerability, pharmacokinetics, and immunogenicity of the therapeutic monoclonal antibody mAb114 targeting Ebola virus glycoprotein (VRC 608): an open-label phase 1 study. Lancet. 2019;393(10174):889-898. doi:10.1016/S0140-6736(19)30036-4
- History of Ebola virus disease (EVD) outbreaks. CDC. Updated March 8, 2021. Accessed April 29, 2021. https://www.cdc.gov/vhf/ebola/history/chronology.html
- Lee A. Ansuvimab: first approval. Drugs. 2021;81(5):595-598. doi:10.1007/s40265-021-01483-4


Comments
Post a Comment