Epidemics have happened before and they’ll happen again. What will we remember? - Science News Magazine
The emergency hospital, a partially demolished building hastily enclosed with wooden partitions, was about to open. It was the fall of 1918 in Philadelphia, and influenza was spreading fast. With many of the city's doctors and nurses serving in World War I, 23-year-old Isaac Starr and his third-year classmates at the University of Pennsylvania School of Medicine needed to help tend the sick. They'd had just one lecture on influenza. Their first job was to assemble the hospital beds, about 25 to a floor.
Starr's shift was 4 p.m. to midnight. The beds soon filled with patients who had fevers, he recalled in a 1976 essay for Annals of Internal Medicine. Many who developed influenza recovered. But Starr witnessed some patients become starved for air, their skin turning blue. Soon, they were "struggling to clear their airways of a blood-tinged froth that sometimes gushed from their nose and mouth," he wrote. "It was a dreadful business."
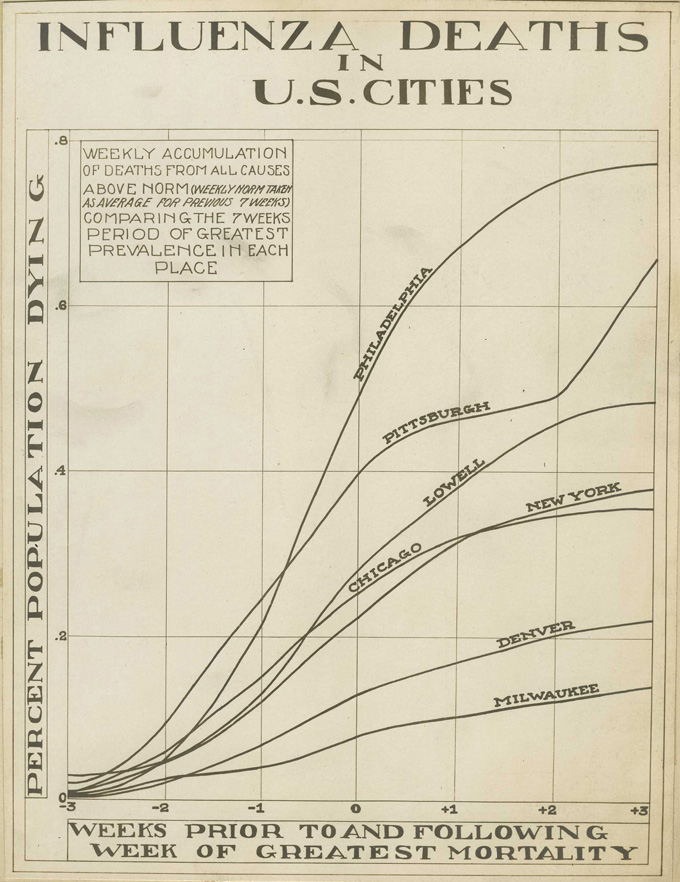
There were no effective treatments. Patients, desperate for breath, became delirious and incontinent and would die within days. "When I returned to duty at 4 p.m., I found few whom I had seen before," Starr wrote. "This happened night after night." In October, around the pinnacle of the pandemic, roughly 11,000 Philadelphians perished.
Some who died in the makeshift hospital stuck with Starr. There was Mike the piano mover, who in a frenzy left his bed and was about to leap from a window before medical staff grabbed him. Mike died shortly after. There was the young woman, "flushed with fever," whose large family kept vigil at her bedside, hoping for a recovery that never came.
An estimated 50 million people worldwide died of influenza during the 1918 pandemic. The century since has seen many vaccines and treatments become available to combat infectious diseases. But beyond those medical feats, the story of epidemics remains a story about people: people who become sick, people who die, people whose lives are upended, people who care for others. And ultimately, people who remember what happened and people who forget.
The public memory of the 1918 pandemic, which lasted into 1919, faded quickly in the United States, with few historical accounts or memorials to victims in the aftermath. One of the first major histories of the pandemic, by Alfred Crosby, didn't arrive until 1976, the same year Starr published his reflections on serving in an influenza ward. Crosby's book was eventually reissued with the fitting title America's Forgotten Pandemic: The Influenza of 1918.
Since 1918, we have faced many epidemics, but COVID-19 has been the first to rival the great flu in how it has changed everyone's daily lives. "We are living through a historic pandemic," says Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases in Bethesda, Md.
But a hundred years' worth of advances in virology, medical understanding and vaccine development has made a difference. It was 11 months from the discovery of the SARS-CoV-2 virus to "having a vaccine that you could put in people's arms," Fauci says, "a beautiful testimony to the importance of investing in biomedical research."
The COVID-19 pandemic is also a stark reminder of what hasn't changed. "Pandemics just surface all the muck," says internist, medical humanities scholar and historian of medicine Lakshmi Krishnan of Georgetown University in Washington, D.C. Ever present but often ignored societal inequities become unavoidable. The disproportionate weight of COVID-19 disease and death on Black, Latino and Native American communities in the United States — "we better not forget," says Fauci. "We really need to address the social determinants of health that lead to these very, very obvious disparities."
Yet outbreak after outbreak, our collective memory falters. The urgency of the predicament eventually fades. The families mourning the loss of loved ones, people struggling with unmet medical needs, with stigma, become small islands of remembrance ever threatened by vast seas of forgetfulness and indifference.
Sometimes forgetfulness comes from a lack of reckoning. The United States moved on from the 1918 pandemic without addressing what was lost. Sometimes the success of vaccines obscures their power. The fear that surrounded polio subsided in the United States after the country rolled up its sleeves for polio vaccines. The dread of many other childhood illnesses, such as diphtheria and measles, has also diminished, leaving some to take prevention measures for granted.
To look back at infectious diseases since 1918 is to observe what we've learned about the viruses, bacteria and fungi with which we share our world, and observe the strides made in lessening their harms. But it's also a call to listen to the stories of how infectious diseases have shaped people's lives.
Outbreaks "have occurred throughout history and they occur now," Fauci says. "And they will continue to occur."
Vaccine victories
On February 24, 1947, Eugene Le Bar, an American merchant, boarded a bus in Mexico City. During the trip, his head began to ache and he broke out with a rash. He arrived in New York City on March 1 still not feeling well. Four days later, he was admitted to the hospital. His stay overlapped with a mumps patient named Ismael Acosta and a little girl, almost 2, who had croup.
Le Bar deteriorated while doctors searched for a diagnosis. He died March 10. Acosta and the little girl had been discharged, but returned later in March with rashes. The results of tests for those two led to a review of Le Bar's autopsy. The diagnosis was smallpox, a disease that kills about 30 percent of those sickened and leaves survivors disfigured by prominent scars.
More victims turned up. A little boy with whooping cough who had been at the hospital developed a rash. So did Acosta's 26-year-old wife, Carmen, who died days later. Soon the number of people with smallpox reached 12. New York City embarked on a massive vaccination campaign.
At the time, Anthony Fauci was 6 years old, growing up in Brooklyn. He remembers his parents talking about a huge event that would be happening in the city. "We all had to get vaccinated, and vaccination means somebody would get a little needle and prick it multiple times in your arm." (The smallpox vaccine wasn't given as a shot; instead, a drop of vaccine was placed on the skin and a needle poked the skin repeatedly to usher the vaccine into the body.) Fauci and his family were among the millions of New Yorkers immunized that spring, bringing the smallpox outbreak to a close without another person added to the count.

Throughout history, smallpox was one of the most feared infectious diseases. A British historian, writing about the 1694 death of Queen Mary II from smallpox at age 32, described the disease as "always present, filling the churchyards with corpses, tormenting with constant fears all whom it had not yet stricken, leaving on those whose lives it spared the hideous traces of its power."
Smallpox is also a starring character in the story of vaccines. At the end of the 18th century, the English physician Edward Jenner extracted fluid from a sore caused by cowpox on a dairymaid's hand and inoculated a young boy with it, a test of the belief among some farmers that getting sick with cowpox protected against smallpox. The experiment propelled forward the concept of vaccination. By giving the immune system a preview of the pathogen, the body's defenses were prepared for the main event.
What followed exemplifies the fullest power of vaccination. After a worldwide campaign, smallpox was the first infectious disease to be declared eradicated from the globe, in 1980 (SN: 11/03/79, p. 310). A scourge that had plagued humankind for at least 3,000 years was consigned to the history books.
Other vaccine-preventable diseases — especially those that afflict children — harm many fewer around the world today than in the near past. During the 20th century in the United States, after vaccines became widely used for nine diseases, including polio, measles and Haemophilus influenzae type b, cases declined by 95 to 100 percent. Yet there can be "a lack of appreciation for what vaccines have done in terms of getting rid of or managing many infectious diseases," says virologist A. Oveta Fuller of the University of Michigan in Ann Arbor.
For many people today, an understanding of polio only comes from history books (SN: 1/20/51, p. 42). But others who grew up when summers meant polio outbreaks have sharp recollections.
Paul Offit, a pediatric infectious disease specialist at Children's Hospital of Philadelphia, was 5 years old in 1956. After surgery on his foot, he stayed for about six weeks in a Baltimore hospital's chronic care facility. It was primarily a polio ward. He was surrounded by children whose limbs were suspended in traction or whose bodies were swallowed in iron lungs.
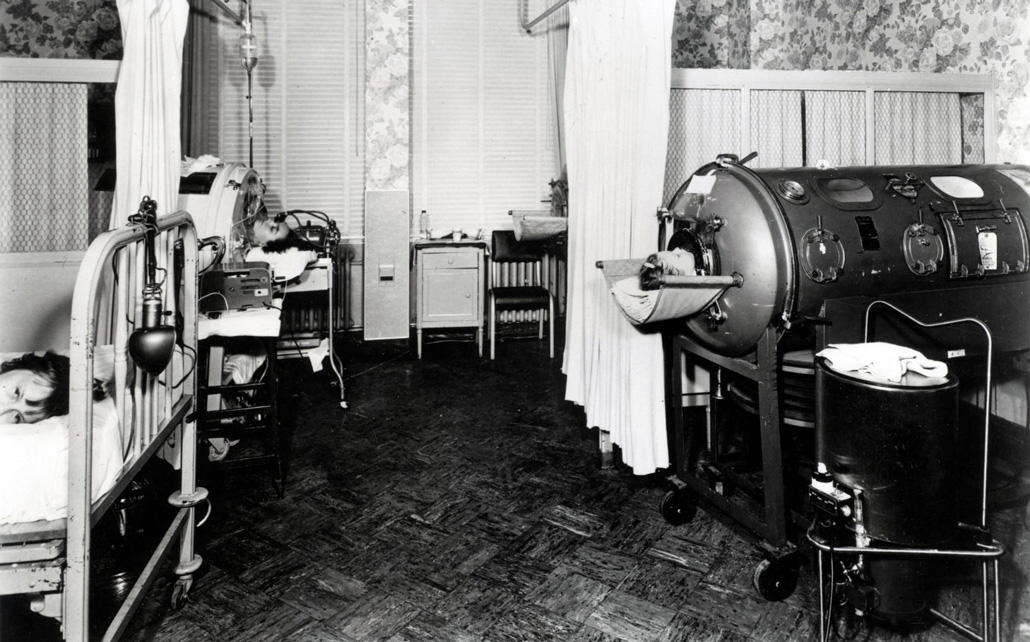
"It was a lonely, frightening experience," Offit says. Parents were allowed to visit only one hour a week. He could see "how vulnerable and helpless and alone all of those children were." Offit's bed was next to a window, which gave him a view of the building's front door. He'd stare at the entrance, "waiting for someone to come save me."
Offit later trained at that same hospital as a medical student. The ward he had languished in as a child was now a suite of offices. The room looked the same, even the molding, "and that window was still there," Offit says. "I remember walking up and looking out that window and seeing the same thing I saw 20 years earlier and just fighting back tears."
Memorial Day weekend in the United States used to herald a season of polio fear, as cases rose in summertime. Children were barred from swimming pools and crowds. Fauci's parents wouldn't allow him and his sister to go to the beach at Coney Island. "All of us as kids knew somebody who'd been paralyzed," says David Morens, Fauci's senior scientific adviser, who grew up in the 1950s.
Vaccines provided an exit from this recurring nightmare. The two vaccines developed to thwart polio each drew on different advances. First came Jonas Salk's "killed" polio vaccine, approved in 1955 (SN: 4/16/55, p. 242). Made with poliovirus that had been treated with formaldehyde, the virus could no longer cause harm, but the body could still mount an immune response against it. About seven decades earlier, Louis Pasteur had demonstrated that rabies virus could be inactivated to develop a rabies vaccine.
The second vaccine, Albert Sabin's oral polio vaccine, became available in 1961 (SN: 12/14/63, p. 370). Often delivered on a sugar cube, Sabin's easily digested vaccine was the inspiration for the song "A Spoonful of Sugar" in the movie Mary Poppins. Sabin's approach was to weaken the poliovirus by making it replicate in nonhuman cells. Forced into an unfamiliar environment, the virus made genetic changes that diminished its ability to cause disease. This method, called attenuation, had first been used about 25 years earlier to create a yellow fever vaccine.

Vanishing ailments
Life before and after polio vaccines was like night and day. In 1952, polio paralyzed more than 21,000 people in the United States. Thirteen years later, that number had plummeted to 61. By 1979, polio was eliminated in the country. With new immunizations, one by one, common childhood ailments all but vanished in the United States: measles, rubella, chicken pox, and meningitis caused by bacteria.
When Kathryn Edwards trained in pediatrics in Chicago in the mid- to late 1970s, "we were really in the grips of Haemophilus influenzae meningitis." (H. influenzae, formerly Bacillus influenzae, is the misnamed bacterium that had once been suspected of causing influenza.) She remembers seeing four or five children at a time hospitalized with this dangerous swelling of the membranes covering the brain and spinal cord, says Edwards, an infectious disease pediatrician and vaccine researcher at Vanderbilt University School of Medicine in Nashville. Some children with H. influenzae meningitis were left with brain damage, while about 5 percent died. Edwards still remembers a young patient lost to the disease the last night of her training.
The first vaccine against H. influenzae type b, the type that most commonly caused meningitis and other severe infections, became available in the United States in 1985. More effective vaccines came a few years later, evaluated by Edwards and colleagues. Again the impact was unmistakable. Before 1985, close to 20,000 children, most of them under age 5, developed severe infections from H. influenzae type b each year, including 12,000 with bacterial meningitis. By 1994 and 1995, the incidence of severe disease had fallen 98 percent in children age 4 or younger. With the availability of vaccines against H. influenzae and other pathogens, "the practice of pediatrics is much different now than when I began 40 years ago," Edwards says.
The scope of infectious diseases that children face worldwide is slowly changing too. From 2000 to 2018, 23 million deaths globally were prevented by measles vaccination. But there are still millions of children around the world missing out on basic immunizations that are routine in the United States. The COVID-19 pandemic has worsened the problem: An estimated 23 million children worldwide did not receive childhood vaccines in 2020; that's about 3.7 million more than in 2019.
The work of developing vaccines against COVID-19 began shortly after researchers worked out the genetic sequence of the new coronavirus, SARS-CoV-2, in January 2020. Previous studies of the coronaviruses behind Severe Acute Respiratory Syndrome, or SARS (SN: 3/29/03, p. 198), and Middle East Respiratory Syndrome, or MERS (SN: 5/31/14, p. 6), had identified a viral protein that would effectively ramp up an immune response.
And the basic research that would underpin a new vaccine technology, which would be used for two of the first COVID-19 vaccines, had been going on for decades. The approach is based on messenger RNA, or mRNA, which carries out of the cell nucleus the instructions for making a protein. The vaccines have the guide for the viral protein; the body makes that protein and produces antibodies against it. Some of the crucial work, modifying the instructions for the viral protein so the body wouldn't see the guide as an invader, came from RNA biologist Katalin Karikó, immunologist Drew Weissman and colleagues working at the University of Pennsylvania Perelman School of Medicine in the mid- to late 2000s.
COVID-19 vaccines were created and tested in the shortest timeline for any vaccines yet. But that efficiency wasn't matched in the distribution. While there haven't been enough shots available globally (SN: 3/27/21, p. 6), the United States, a country awash in supply, has struggled to immunize everyone eligible. Some people haven't been vaccinated because they can't take time off work to recover from side effects or are worried they'll have to pay for the shots. Others don't see COVID-19 as a threat and don't see the need for the vaccine.
COVID-19 has killed millions of people worldwide. Yet perhaps it would be more terrifying if it primarily threatened children. The horror of polio was that it could leave children paralyzed for the rest of their lives, Offit says; it was as though children had been injured in war.
Michigan's Fuller thinks that seeing the harm that polio could do to children helped make Americans eager for polio vaccines. During the COVID-19 pandemic, "because we were all isolated, we didn't see each other really suffering or dealing with the effects of this virus," she says.
One person vaccinated feels like such a victory.
Katherine Spindler
When virologist Katherine Spindler of the University of Michigan was growing up, she had measles, mumps and rubella. The vaccines for those afflictions "came along too late for me," Spindler says. She still remembers the name of her older brother's classmate who died in eighth grade of an infectious disease. The routine immunizations that are now regular parts of pediatrician appointments mean that most of us "don't know what it's like to have polio or to die from measles."
Spindler found getting the COVID-19 vaccine "so meaningful," thinking about all of the science that came together to develop it. People have e-mailed her with questions about the vaccine. One woman who had an appointment but wasn't sure she wanted to keep it wrote several times. Spindler spent a few hours responding. Finally, she got an e-mail back with a picture of the woman in her car getting the shot. "Tears came to my eyes," Spindler says. "One person vaccinated feels like such a victory."
The aftermath
At the start of the COVID-19 pandemic, Lakshmi Krishnan and S. Michelle Ogunwole were internists at Johns Hopkins Hospital in Baltimore. Patients were dying. There wasn't enough personal protective equipment for staff. So much about COVID-19 was still unknown. "It was terrifying," says Krishnan, now at Georgetown University. Some of her colleagues were writing their wills.
And the patients were largely alone. Ogunwole, also a health disparities researcher at Johns Hopkins University School of Medicine, remembers an older Black woman who had been hospitalized with COVID-19 for months. She was well enough to move out of the intensive care unit but was extremely debilitated because she hadn't walked in so long, Ogunwole says. A tube in her windpipe made talking difficult as well.
The woman's family was not there. "There was nobody to speak for her," Ogunwole says. It made Ogunwole think of her own mother, "an incredibly vibrant person … the life of the party." If it was her mom in that bed, no one would have known who she is. That she likes to dance for no reason. That she picks up a different sport every year.

Ogunwole felt her patient's sorrow and loss. Millions are reckoning with the pandemic's cost to their physical and mental health. The toll is not unlike that of tuberculosis, AIDS, fungal diseases, childhood infectious diseases or the many other outbreaks and epidemics of the last century.
We should know by heart how lives — and whose lives — are changed by infectious disease outbreaks. But time and again, there's a clamor to leave outbreaks behind us. And the trauma and the inequities linger. The question this time, says historian Nancy Bristow of the University of Puget Sound in Tacoma, Wash., is, "Can we do a better job of continuing to hear the stories of those who have been affected?"
The stories of children who have lost one parent or both, for example. For her book American Pandemic: The Lost Worlds of the 1918 Influenza Pandemic, Bristow interviewed Lillian Kancianich, born in a small town in North Dakota. Kancianich's mother died of influenza when Kancianich was a baby. The story was that her mother was out sweeping the porch on Armistice Day and then was never seen again, Bristow says.
Kancianich bounced among extended family members' houses for two years before she was able to call one home. She told Bristow that as a child, when asked what she wanted to be when she grew up, her answer was, a stepmother. "The loss of that parent changed her life completely," Bristow says.
These stories have continued. In roughly the first year of the COVID-19 pandemic, an estimated 1 million children worldwide experienced the death of a mother, a father or both, researchers reported in July in the Lancet. The number is staggering, and yet it is a fraction of the estimated 17 million children who have lost one or both parents to AIDS in roughly the last three decades, according to the United States Agency for International Development. Ninety percent of those children live in sub-Saharan Africa.
Outbreak after outbreak, our collective memory falters. The urgency of the predicament eventually fades.
Nearly 105,000 children in the United States are facing life without one or both parents due to COVID-19, the study in the Lancet found. "Evidence from previous epidemics shows that ineffective responses to the death of a parent or caregiver, even when there is a surviving parent or caregiver, can lead to deleterious psychosocial, neurocognitive, socioeconomic and biomedical outcomes for children," the authors wrote.
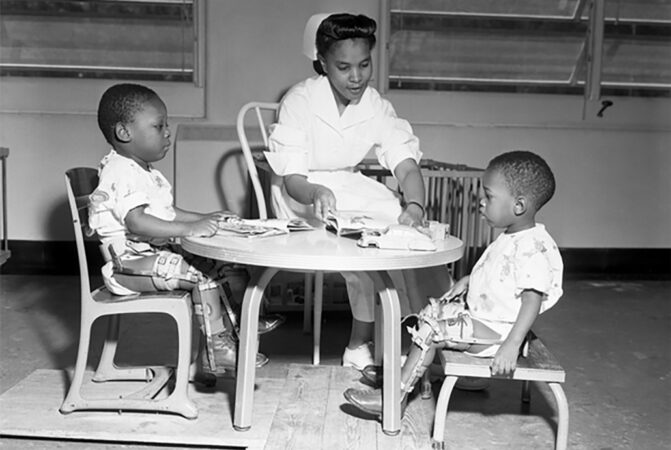
An earlier study on parental death due to COVID-19 in the United States took race and ethnicity into account. While Black children make up only 14 percent of children in the United States, they made up 20 percent of those who had lost a parent, researchers reported in April in JAMA Pediatrics.
When Krishnan was treating patients early in the pandemic, she remembers noting, "It's all my Black and brown patients that are getting upgraded to the intensive care unit." Research has revealed a disproportionate impact among Black, Latino and Native Americans in terms of infection, hospitalization and death.
"COVID has unveiled disparities in health," but the pandemic didn't create them, Fuller says. "This is not new."
At the turn of the 20th century, Black Americans' death rates were higher than white Americans for tuberculosis, pneumonia and, in children, diarrheal disease and diseases of malnutrition, W.E.B. Du Bois wrote in 1906, "an indication of social and economic position." Racism and segregation restricted access to health care, housing and wealth for Black Americans.
The accounts from 1918 in Black newspapers in Philadelphia and Chicago "gave the impression that the epidemic did not substantially disrupt life in black communities," wrote Vanessa Northington Gamble in Public Health Reports in 2010. Yet it was clear that the number of Black people who did have flu "overwhelmed the medical care facilities that were available to them," says Northington Gamble, a physician and medical historian at George Washington University in Washington, D.C. White hospitals wouldn't accept Black patients or would send them to the basement or other segregated areas. Black hospitals didn't have the capacity for everyone who needed care. So Black communities came together to provide for their own, she says.

When every one of the 75 beds at Frederick Douglass Memorial Hospital in Philadelphia filled up, its medical director, with no support from the city's board of health, managed to open an emergency annex for Black patients. Black women volunteers in Chicago made house visits to tend to the sick.
Black nurses also cared for Black influenza patients in their homes. Bessie B. Hawes, a 1918 graduate of the Tuskegee Institute's nursing program, described her experience caring for a family of 10, "dying for the want of attention," in a rural area of Alabama. "As I entered the little country cabin, I found the mother dead in bed, the father and the remainder of the family running temperatures of 102 to 104˚. Some had influenza and others had pneumonia…. I saw at a glance that I had much work to do…. I milked the cow, gave medicine, and did everything I could to help conditions."
One of the legacies of the 1918 pandemic is "this long-standing tradition of the Black community of standing up and taking care of itself," says Northington Gamble. The tradition continues, she says, with the work of organizations including the Black Doctors COVID-19 Consortium, created to make it easier for Black communities in the Philadelphia area to receive COVID-19 testing and vaccination.
When Black people became ill with influenza in the 1918 pandemic, they were more likely to die than white people with influenza, researchers reported in 2019 in the International Journal of Environmental Research and Public Health. That higher likelihood of death "could be attributed to several factors still present today: higher risk for pulmonary disease, malnutrition, poor housing conditions, social and economic disparities, and inadequate access to care," Krishnan, Ogunwole and their colleague Lisa Cooper of Johns Hopkins University wrote last year in Annals of Internal Medicine.
The societal systems that foster racial discrimination and lead to health inequities must be addressed, Ogunwole says. "There is no amount of resilience that overcomes that."
We cannot forget because it will happen again.
Lakshmi Krishnan
The suffering of the 1918 pandemic was overshadowed by the end of World War I, Bristow says. The war was publicly memorialized with monuments and a holiday. "The pandemic goes unspoken," she says, because it doesn't fit with the victorious narrative of the war. Only a few fictional works that drew upon the 1918 pandemic were published in the following decades.
But those books — such as the 1939 Pale Horse, Pale Rider, by Katherine Anne Porter, who survived an influenza illness but whose fiancé died — as well as private letters reveal deep loss, Bristow says.
"It's very clear that the trauma stayed with people, even if there's not public grieving, and that's what's so sad about it," she says. "There was no public acknowledgment of all of this loss." The country marched ahead, and people "were expected to hop in line and march along too."
Krishnan, a historian of medicine, says we must preserve a record of the COVID-19 pandemic. A hopeful sign that stories of how people felt, lived, loved and died won't be lost are the many oral history projects spearheaded by universities and libraries. "We cannot forget," Krishnan says, "because it will happen again."



Comments
Post a Comment